Breastfeeding is a vital aspect of newborn care, providing essential nutrients, antibodies, and promoting a strong bond between mother and child. However, in cases where a newborn is diagnosed with jaundice, concerns often arise regarding the safety and efficacy of breastfeeding. Jaundice, characterized by elevated levels of bilirubin in the blood, can cause a range of symptoms from mild yellowing of the skin and eyes to more severe complications if left untreated. The primary concern with jaundice in newborns is the potential for bilirubin to reach toxic levels, leading to kernicterus, a form of brain damage. Understanding the relationship between breastfeeding and jaundice is crucial for managing the condition effectively while supporting the health and well-being of both mother and baby.
Understanding Jaundice and Breastfeeding

Jaundice is common in newborns, affecting approximately 60% of term babies and 80% of preterm infants. It typically presents within the first week of life, peaking around the third to fifth day. Breast milk jaundice, a specific type of jaundice, occurs in some breastfed babies due to substances in the breast milk that can increase the reabsorption of bilirubin from the intestines. Despite this, the benefits of breastfeeding for both the mother and the baby generally outweigh the risks associated with jaundice. Breast milk provides optimal nutrition, enhances the baby’s immune system, and supports cognitive development. Furthermore, breastfeeding can help in the management of jaundice by ensuring adequate hydration and promoting the excretion of bilirubin through stool.
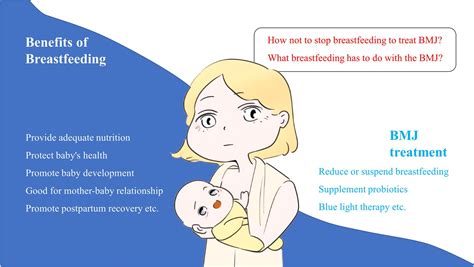
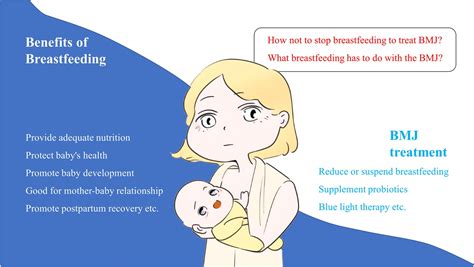
Benefits of Breastfeeding in Jaundice Management
While it might seem counterintuitive, breastfeeding is not only safe but also recommended for babies with jaundice. The primary benefits include:
- Adequate Hydration: Breast milk is rich in water content, helping to keep the baby hydrated, which is essential for the excretion of bilirubin.
- Enhanced Bilirubin Clearance: Frequent bowel movements stimulated by breast milk help in the elimination of bilirubin from the body.
- Optimal Nutrition: Breast milk provides all the necessary nutrients for the baby’s growth and development, even when they are undergoing treatment for jaundice.
- Immune System Support: The antibodies in breast milk support the baby’s immune system, reducing the risk of infections that could complicate jaundice.
It is essential to note that the decision to continue breastfeeding should be made in consultation with a healthcare provider. In some cases, temporary cessation of breastfeeding may be advised to assess whether breast milk is contributing to the jaundice. However, this should be a last resort and typically under close medical supervision.
| Type of Jaundice | Description | Prevalence |
|---|---|---|
| Physiological Jaundice | Common, mild jaundice peaking at 3-5 days | Affects approximately 60% of term babies |
| Breast Milk Jaundice | Jaundice in breastfed babies due to breast milk components | Affects a smaller percentage of breastfed babies |
| Pathological Jaundice | Jaundice presenting within the first 24 hours or persisting beyond 2 weeks | Less common, often requiring medical investigation |

Key Points
- Jaundice is common in newborns and can be managed with proper care and monitoring.
- Breastfeeding is recommended for babies with jaundice due to its nutritional and hydrating benefits.
- Breast milk jaundice is a specific type of jaundice that occurs in some breastfed babies.
- Adequate hydration and frequent bowel movements are crucial in the management of jaundice.
- Close medical supervision is necessary to determine the best course of action for managing jaundice in breastfed babies.
Monitoring and Treatment of Jaundice
The management of jaundice involves regular monitoring of bilirubin levels, typically through blood tests, and ensuring the baby remains well-hydrated. In cases where bilirubin levels are elevated, phototherapy may be recommended. This involves exposing the baby to special lights that help break down bilirubin in the skin. In severe cases, exchange transfusions may be necessary to rapidly reduce bilirubin levels. It is crucial for parents to work closely with their healthcare provider to monitor the baby’s condition and adjust the treatment plan as necessary.
Role of Parents and Healthcare Providers
Effective management of jaundice requires a collaborative approach between parents and healthcare providers. Parents should be educated on the signs of jaundice, the importance of breastfeeding, and how to monitor their baby’s condition. Healthcare providers must provide guidance on breastfeeding, offer support, and closely monitor the baby’s bilirubin levels and overall health. Regular follow-up appointments are essential to adjust the treatment plan according to the baby’s response and to address any concerns the parents may have.
In conclusion, breastfeeding plays a critical role in the management of jaundice in newborns. While it is essential to monitor bilirubin levels closely and manage jaundice appropriately, the benefits of breastfeeding should not be overlooked. With proper care, support, and medical supervision, most babies with jaundice can thrive and develop normally.
Is it safe to breastfeed a baby with jaundice?
+Yes, breastfeeding is not only safe but also recommended for babies with jaundice. It provides essential nutrients and helps in the excretion of bilirubin.
What are the signs of jaundice in newborns?
+Signs of jaundice include yellowing of the skin and eyes, which can be more noticeable in the gums, nose, and soles of the feet. Other signs may include lethargy and poor feeding.
How is jaundice treated in newborns?
+Treatment depends on the level of bilirubin and the baby’s overall health. It may include phototherapy, hydration, and in severe cases, exchange transfusions.
Can breastfeeding cause jaundice in babies?
+Breast milk jaundice can occur in some breastfed babies due to substances in the breast milk. However, this is different from breastfeeding causing jaundice. The benefits of breastfeeding generally outweigh the risks.
How often should bilirubin levels be checked in a baby with jaundice?
+The frequency of checking bilirubin levels depends on the baby’s age, the level of bilirubin, and the presence of other risk factors. This should be determined in consultation with a healthcare provider.